Flu season is here. The summer wave of the coronavirus has receded, but the winter uptick is probably around the corner. Shots are available for both respiratory viruses, raising questions about the best time to get these shots if you haven’t had one already.
The Washington Post spoke to two infectious-disease experts about how they make their own decisions and how they talk about these issues with friends and family.
Caitlin Rivers, an infectious-disease epidemiologist and senior scholar at the Johns Hopkins Center for Health Security, is a 35-year-old mother of an 11-year-old and 6-year-old twins. She also writes a weekly newsletter that tracks covid, influenza, RSV and food recalls. Andrew Pavia is a 69-year-old pediatrics infectious-disease physician at the University of Utah.
Explore More
Here’s what they said:
Rivers’s decision: Rivers, her husband and three school-age children always get both shots, typically by the end of October, because once her children are back in school, they tend to become sick and bring germs home. Even though they are young, healthy and at low risk for severe disease, getting the shots protects her family from missing work and school, she said.
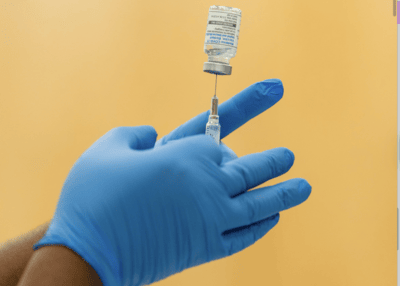
For convenience, one twin received her coronavirus shot earlier this month, when the pediatrician offered it during a visit. The rest of the family got their shots Tuesday at a pharmacy because they received a text reminder. The vaccines do not do much to prevent infection, but they reduce symptoms and prevent severe illness, she said. The coronavirus vaccine also reduces the risk of long covid, for which symptoms such as brain fog and severe fatigue persist or newly develop more than three months after a coronavirus infection.
Pavia’s decision: Pavia, who is in a higher-risk age group, usually gets both shots in October. He got his flu shot in early October because it was offered at work and was convenient. He got his coronavirus shot recently, after it became clear he could get it free at a pharmacy following recent confusion about federal recommendations. Pavia still sees patients, including children with weak immune systems, and is around elderly and frail adults who could much more easily get sick and die, he said.
Here are some of their tips for Americans on vaccination strategy.
What matters: Timing or convenience?
Pavia encourages getting a shot whenever you have an easy opportunity. If you’re getting groceries and the pharmacy is offering flu shots, take five minutes to get one, because you are less likely to follow through by scheduling an appointment, Pavia said.
The Centers for Disease Control and Prevention now recommends that people consult a clinician before receiving a coronavirus shot, but that process can be as simple as a brief conversation with a pharmacist. The Post previously published a guide to getting covid shots under these new conditions.
Get them together or separate?
By now, many people know how they react to flu and coronavirus shots. The coronavirus shot can give some people quite a sore arm. If that’s the case, avoid getting both shots in the same arm, they said. Rivers got her shots in two different arms during the same visit, but the rest of her family got them in the same arm. For people who don’t have much a reaction, there is no disadvantage to getting two shots at the same time, Pavia said. He got his shots at different times because that’s when it was convenient for him.
Which version of the covid shot to get?
People who have had a strong reaction to the Pfizer and Moderna mRNA shots might consider the Novavax vaccine, which uses a more traditional protein-based technology, as an alternative for fewer temporary side effects, they said.
For males between 12 and 29, it may make sense to get the Novavax vaccine, because there is no known risk of myocarditis, a rare condition that causes inflammation of the heart muscle, Pavia said. That is a known but rare side effect of mRNA vaccines, although health officials have stressed that the cases are generally mild and that the covid disease itself carries a greater risk of heart complications.
There are no major differences between the Moderna and Pfizer vaccines, Pavia said. Both he and Rivers get whichever is more convenient. Rivers said she doesn’t even ask which brand she is getting.
When do coronavirus vaccines wear off?
There is no absolute answer for how long protection lasts. For most people, protection from infection is pretty good for six months, Pavia said.
Those at highest risk should consider two shots a year, because protection fades faster the older you are, and the risk of complications goes up, Pavia said.
“But I don’t agree that everyone over 65 absolutely needs a booster every six months,” he said. “If you are generally healthy and had frequent boosting from infection and vaccines, that may not be necessary.”
Regardless of risk factors, Pavia
said, people can time vaccination ahead of major events such as weddings or conferences. The immune response does not fully kick in for about two weeks, and peaks at about a month, so people should plan ahead if they want maximal protection, Pavia said.
How to think about flu season
The timing and intensity of flu season varies. Data suggests this year’s season is just beginning, Rivers said.
Flu vaccine effectiveness wanes at five or six months, which is most clearly evident in older adults, Pavia said. That’s why he generally avoids getting a shot in September, but he doesn’t think people should fixate too much on timing. Getting vaccinated in October should provide protection through March, which is when the flu season usually ends. Waiting until around Halloween could stretch out your protection for a late flu season. But by Thanksgiving, flu is usually widely circulating, and it spikes right after the holiday.


